Case Report : 60 year old female with complaints of Shortness of breath and Cough and Comorbidities- Diabetes and Hypertension
Summary :
Then patient was given INJ i.v.adenosine 3mg IV/STAT but rythm not reverted to normal but so 6mg IV adenosine given and it resulted in atrial fibrillation
60 year old female admitted in the hospital with the cheif complaints of shortness of breath, non productive cough and generalised body swelling from 4 days.
Introduction :
60 year old female came to the hospital 4 days back with chief complaints of shortness of breath,non productive cough and generelised body swelling since 2 days.
Pt was asymptomatic 8 years back and was a vegetable vendor.Then she developed 4-5 swellings on rt side upper back.She has undergone surgery for the same and was discharged from the hospital after 5 days.She has stopped selling vegetables and would go to the farm weekly 3-4 days.
She was taken to the hospital 3 years back with complaints of generalised weakness and was diagnosed with Diabetes mellitus and Hypertension and started using Glimi M1 And Nifedipine medication.
Then 15 months back she had swelling of the face,upper and lower limbs and pt was unable to speak but no problem with limb movement and bowel and bladder movement.Then she was taken to Devarakonda private hospital and according to the patient attender she was given an injection and swelling decreased within 1-2 days.Then she returned home and was continuing with Diabetes and Hypertension medication.After 4-5 months she was also diagnosed with Hypothyroidism and was using Thyoroxine 50micrograms from then.
Then from 3 months she has complaints of weakness and sweating and when taken to the govt.hospital in nalgonda attenders were said that she was having hypoglycemia.There were 2 episodes within 3 months.
10 days back again she was having generalised swelling and uncontrolled bowel and bladder movements and she was put in emergency care for 1 day in Nalgonda govt hospital and was discharged from the hospital after 2 days and was taken home.
Four days back she was having sudden onset of SOB at rest,non productive cough and swelling of upper and lower limbs,burning micturition and was taken to Nalgonda govt hospital and was referred to kamineni hospital.
Daily routine :
She wakes at 6 am in the morning finishes her daily chores and eats breakfast and goes to cotton field for work at 9 am taking a lunch box containing rice and vegetablea with her,takes a break in afternoon and returns home at almost 5 pm in evening.
She gets tired by evening smokes one chutta and eats her dinner and sleeps by
10 pm in night.
Her husband has died 10 years back due to which she was unable to go for work for 1-2 months but then she resumed her field work.And again her work has been effected from past 3 months due to weakness.
Dietary habits :
She is a non vegetarian and consumes chicken 1-2 days per week.
She has stopped eating nonveg since 1 year as having tooth ache.
She has habit of smoking 1-2 Chutta every day from the past 20 years which has continued until 10 days back.
Her relatives have asked to stop smoking but she says that her bowel movement will be free by smoking and she thinks that smoking will help in food digestion.
She drinks alcohol occasionally..almost once every 3-4 months.
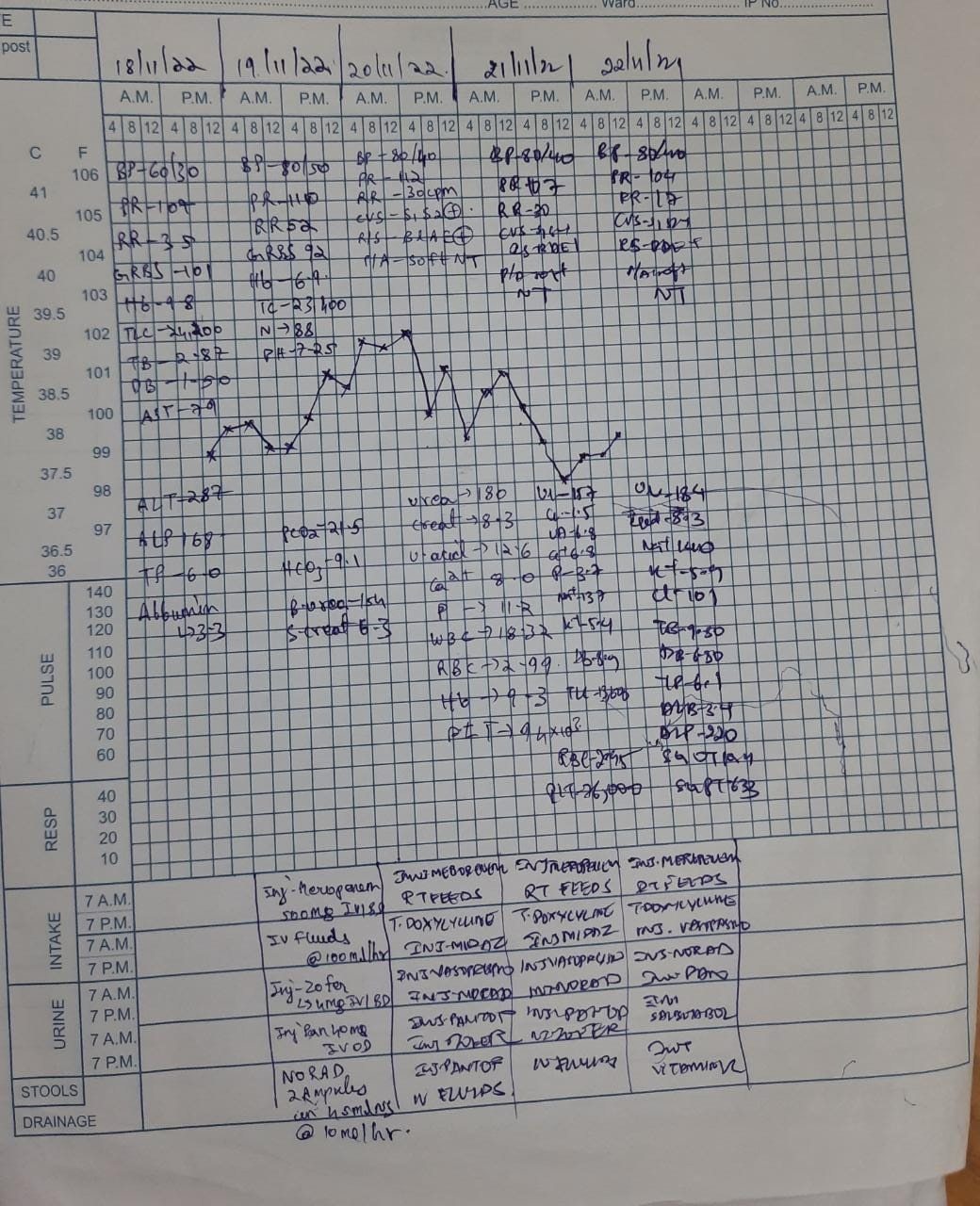
Vitals at the time of admission
Date : 27-04-24
BP : 140/100 mmHg
PR : 113
spO2
Temp
Random Blood Glucose : 196 mg/dl
Patient was drowsy but was answering questions.
Lab reports on the day of admission
( 27-04-24)
Increased Levels of phosphorus along with raised creatinine,urea,uric acid suggests Chronic kidney disease.
BUN/Creat ratio <20 rules out pre renal AKI.
There is loss of albumin in the urine,so there impairment in the renal filtration which may be explained by Chronic diabetes mellitus resulting in Diabetic nephropathy.
Pt was administered Bicarbonate for treating the Metabolic acidosis infered from the above abg report .And then she has undergone Heamodialyis as the metabolic acidosis was resistant to treatment and also the creatinine levels were high.
Protuberant abdomen on examination but no tenderness,rebound tenderness or gaurding.
Usg Abdomen :
Date : 28-04-24
Treatment :
Fluid restriction 1 lit/day
Salt restriction 22g/day
GRBS-147 mg/dl
INJ PIPTAZ 2.25 gm IV/TID
INT LASIX 40mg IV/SD
INJ InsulinS/C TID acc. to GRBS
Tab NICARDIA 20mg PO/TID
Tab NODOSIS 500mg po BD
Tab Thyronorm 50microgram OD
Tab SHELCAL-CT PO OD
Tab OROFER -XT PO -01-x-x
INJ Epo 4000 INJ S/C
INJ IRON SUCROSE 200mg
Decreased heamoglobin may be explained by decreased erythropetin due to decreased renal function.
As Iron levels are also of low normal levels OROFER XT is given as it is required for heamoglobin formation by EPO.
She has undergone Heamodialysis on 28-04-24 as her creatinine levels were still raised.
Date : 29-04-24
Pulmonology referral was done due to presence of diffuse rhonchi
2D Echo :
Patient had tachypnea and was started on non invasive ventilation
Date : 30-04-24
ROSC was achieved by 4:20 am
Patient GCS was low and was having hypoxia, so was intubated.
Post-Intubation ABG
Patient also had Supraventricular tachycardia
Ventilator settings :
FiO2 : 90 %
PEEP : 6cm H2o
VT : 450ml
RR : 14
02-05-24
ABG - Metabolic Acidosis,Type 1 Respiratory Failure.
1 : 30 am
ventilator settings :
FiO2 : 35
PEEP : 6cmH2O
VT : 450
RR : 14b/min.
GCS : E1VtM1
Resp Exmn : B/L Air entry present.
Provisional Diagnosis :
Chronic Renal Failure
Type1 Respiratory Failure
Date 03-05-24 :
Date 04-05-24
Thyronorm dose increased to 100 microgram.
Can Euthyroid sick syndrome be considered ?
Provisional Diagnosis
Chronic Renal Failure
ARDS
Urosepsis?




















































Comments
Post a Comment